A Treatment Protocol for Idiopathic Toe Walking
— Susan Steindorf, MSPT
 Treatment of idiopathic toe walking has been a challenging issue for me; and, in my experience, not treating the source and deficits has resulted in long-term orthopedic and functional problems. In my work as a school pediatric physical therapist, I have recently developed a strategy that works for my patients. Perhaps it can help yours as well. My protocol centers on assessing the toe walking pattern, identifying cause(s) of toe walking, and treating range of motion limitations.
Treatment of idiopathic toe walking has been a challenging issue for me; and, in my experience, not treating the source and deficits has resulted in long-term orthopedic and functional problems. In my work as a school pediatric physical therapist, I have recently developed a strategy that works for my patients. Perhaps it can help yours as well. My protocol centers on assessing the toe walking pattern, identifying cause(s) of toe walking, and treating range of motion limitations.
Assessing the Pattern
First, to identify the source of toe walking, assess the frequency of the toe walking pattern. If the child is almost always up on toes and not able to control the pattern, look closely for a neuromuscular source. Assess tone, active and passive range, and motor coordination, specifically of the ankles. Watch how the child moves and look for patterns from increased tone or weakness.
In most cases, if the source of toe walking is neuromuscular (cerebral palsy or other neurological conditions), then coordination, motor control, and range are affected. If the child has good control of ankle movements within her available range of motion, look for other reasons why the child is toe walking. They do not do this for fun!
If toe walking is intermittent, observe whether there is a pattern to when the child is up on her toes. Often it is connected to when a child is excited, over-stimulated, or fatigued, and the toe walking correlates with sensory processing difficulties. Children will walk on toes in order to get proprioceptive input to try to organize their system.
In cases where this has gone untreated for a long time and the child has lost significant range, she may predominantly walk on toes due to orthopedic limitations.
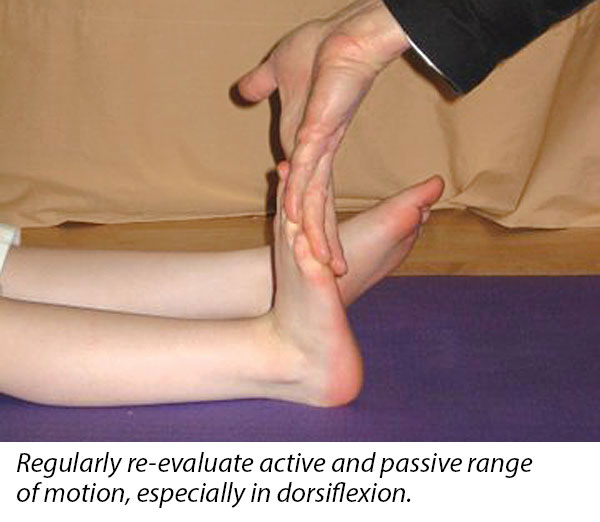
It is critical to measure range of motion and note the resistance necessary to get to the end range. If there is significant resistance, recognize that it will be difficult for her to use her end range functionally.
 Key Issues
Key Issues
Next, discover the issues present that may cause the child’s toe walking. If sensory-seeking behavior is an issue, it’s very important to assess the child’s sensory processing and begin to look at her behavior from this perspective.
Giving the child sensory input and other forms of proprioceptive input is critical to decreasing the sensory-seeking pattern. Have a child play in a way that she gets deep pressure into the joints (for example, jumping or lifting heavy objects). Using a weighted blanket can also help.
It is very important to recognize when a child is overstimulated and to teach calming techniques such as deep breathing and other calming sensory input. A sensory questionnaire and interview with the child and family can often provide valuable information about what input is calming to the child.
Providing sensory input before and during challenging activities or in preparation for stressful environments can help. Essentially, you are providing a sensory “diet” for children with challenges in this area so they can be in an optimal level of alertness during their day. To guide this process, enlist the assistance of someone who is trained to assess sensory processing challenges.
Other issues related to toe-walking may be a neuromuscular defect or a physically shortened gastrocnemius and Achilles tendon. These would require different therapy strategies and are outside the scope of this discussion.
Restoring Range of Motion
As the final piece of the treatment strategy, if there is a loss of range of motion (less than 10 degrees passive and active range), then plan to restore range for function and to preserve the child’s foot structure.
In the challenge of restoring range, the JumpStart®Kangaroo® has been an incredibly effective tool for me. You can’t expect a child to wear the JumpStart Kangaroo during the day if she does not yet have the range to seat the heel comfortably. So, for a prolonged passive stretch, have the patient wear the brace as a night splint. If the child tends to push into plantarflexion and out of the brace, you can add the Kangaroo’s super heel seating strap.
If the child has difficulty with compliance, have her wear one brace at a time on alternate nights. Once range has been restored to at least five degrees past neutral, she can wear the brace during the day to help break the pattern of toe walking. Day use is only necessary if the child continues to toe walk after she has normal range. In my experience, with constant night use for range, it has usually been necessary to use the brace during the day for only a few weeks.
Using the JumpStart Kangaroo for Idiopathic Toe Walking
- Evaluate the pattern.
- Assess key issues.
- Plan the wearing schedule.
Night use - Kangaroo for ROM
When ready for day use - Kangaroo for new pattern. - Re-evaluate.
Suspend day use?
Move to lower level of support for day use?
When ROM is restored, suspend night use?
Moving On
Once range and gait have been restored to normal, you can dismiss the use of the Kangaroo splints. However, it is important to monitor the new abilities. Regression and loss of range can happen, and if this occurs, you can reprise the treatment protocol as needed. The child may not be receiving ongoing therapy, so it is important to educate the family and check in from time to time.
 Susan Steindorf, MSPT, NDT, is a pediatric physical therapist certified in neurodevelopmental treatment who has worked in pediatric hospitals and in the Bainbridge Island (Wash.) school district since 1988. Teaching children a wide range of fitness activities and working with children with special needs as a pediatric PT has been a source of joy and discovery. Susan also teaches yoga to children and adults of all abilities.
Susan Steindorf, MSPT, NDT, is a pediatric physical therapist certified in neurodevelopmental treatment who has worked in pediatric hospitals and in the Bainbridge Island (Wash.) school district since 1988. Teaching children a wide range of fitness activities and working with children with special needs as a pediatric PT has been a source of joy and discovery. Susan also teaches yoga to children and adults of all abilities.