Tibial Varum:
Recognizing its presence and accommodating it in bracing
— Don Buethorn, CPO
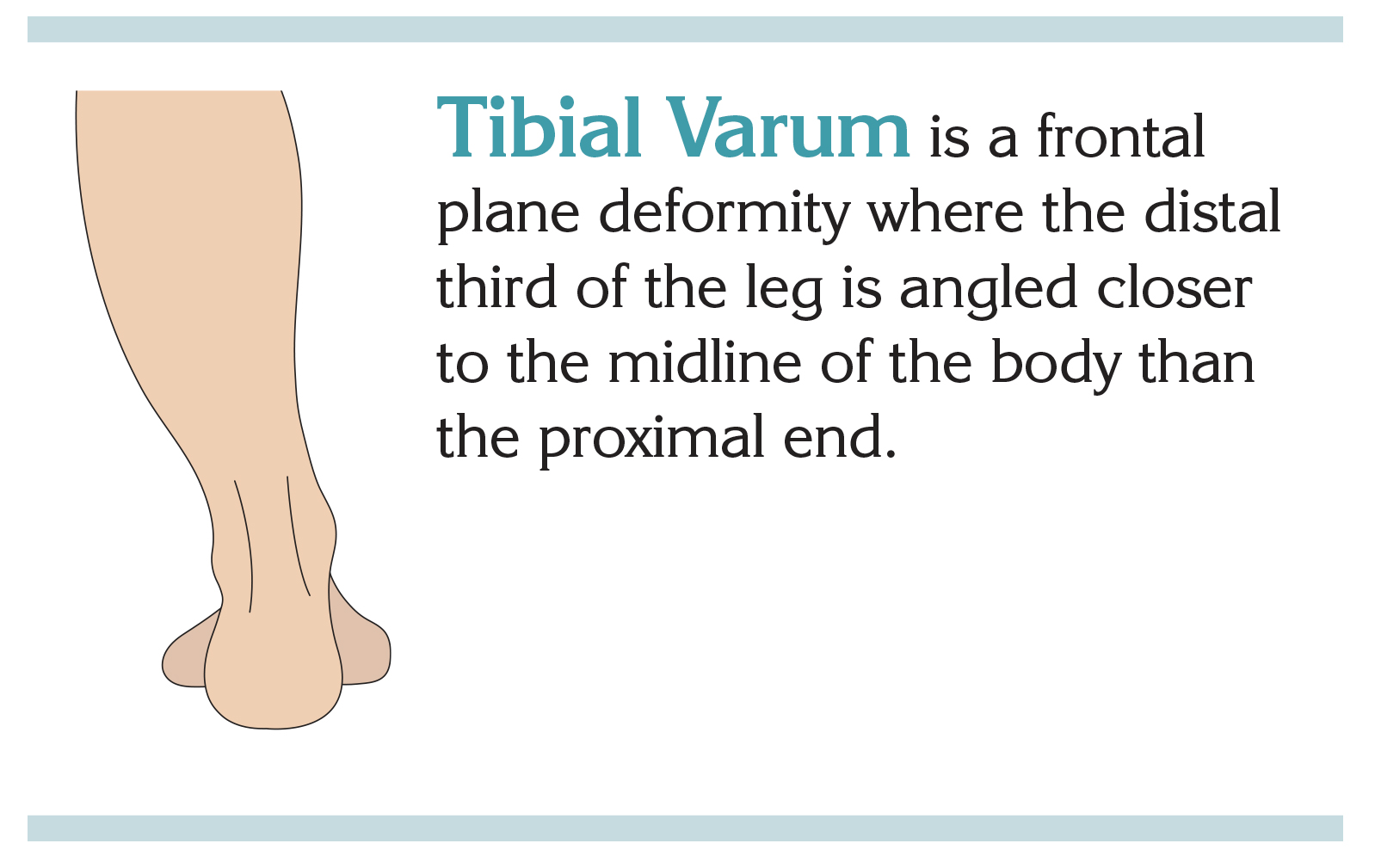
Sometimes patients exhibit mild tibial vara (a bowing deformity of the tibial) or genu vara (a medial angulation of the distal tibial in relation to the thigh). Tibial vara (vara is the plural of varum and is used for bilateral presentation) is a normal frontal plane deformity in children under the age of 2 to 3 years and usually disappears on its own by age 6. It can also be present when the medial proximal tibial growth plate has been disturbed by injury or disease. Mild presentations of tibial varum can be physiologically normal in individual cases. Though more common in a pronating patient, supinators may also exhibit this lateral tibial tilt, as we will see in our patient example. Whenever tibial varum is present, the key is to accommodate it when planning a bracing project.
(Please note that in this article we are not addressing cases of true infantile tibial vara or Blout’s disease where the angle is severe and asymmetric.)
Standard clinical approaches to bracing may run counter-intuitive to finding solutions. The tibial varum issue often goes unnoticed as a source of the problem. When a brace isn’t working and the source of the trouble is hard to trace, tibial varum may be something to consider.
 This article:
This article:
- reviews some relevant background in gait cycle transitions;
- examines how to plan the position of function when tibial varum is present;
- considers a case in point from the Cascade casebook, including an error we caused ourselves;
- summarizes our breakthroughs and findings; and
- offers helpful suggestions for clinicians when casting and ordering braces for patients with tibial varum.
Gait cycle transitions
Consider the gait cycle’s moving center of weight and its effect on the foot. At heel strike, the foot encounters the ground in very slight supination. This triggers an immediate shift toward pronation, absorbing shock and adjusting for uneven terrain. As weight transfers from hindfoot to midfoot, the foot moves into pronation. At mid-stance, the foot is in slight pronation and continues in that direction. In rolling through to toe-off, the ankle transfers weight to the forefoot, with the foot leaving the ground again in supination.
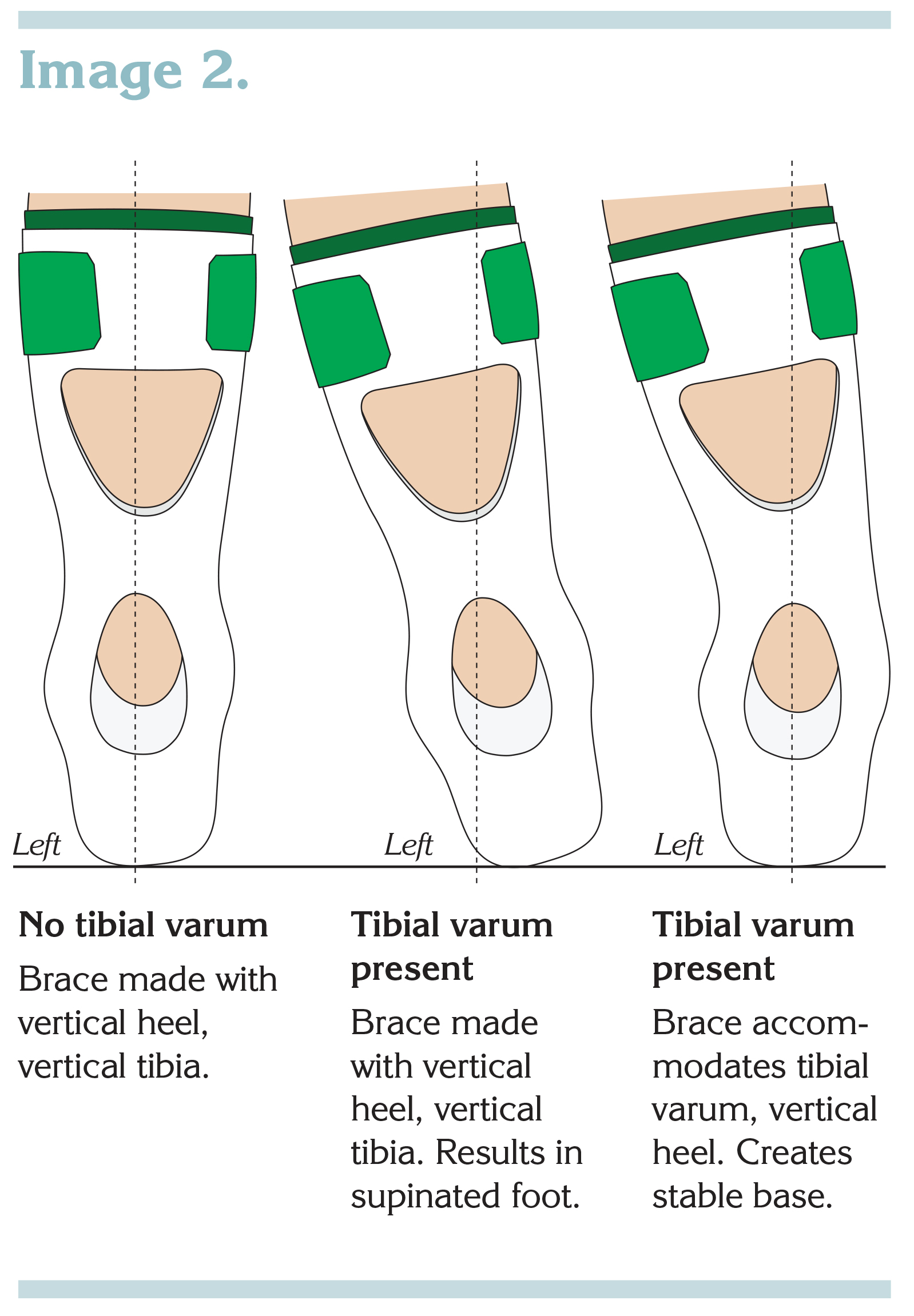
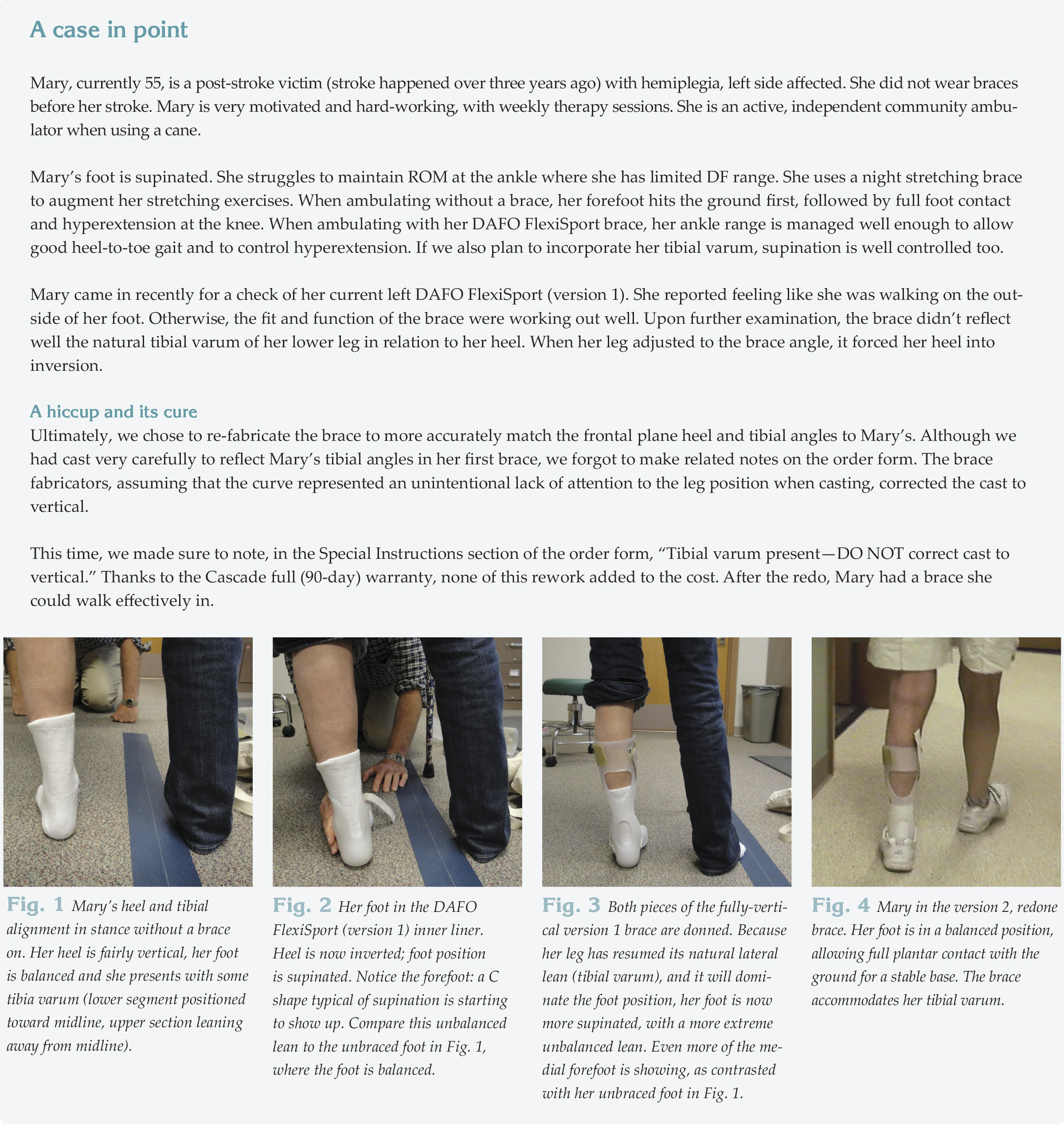
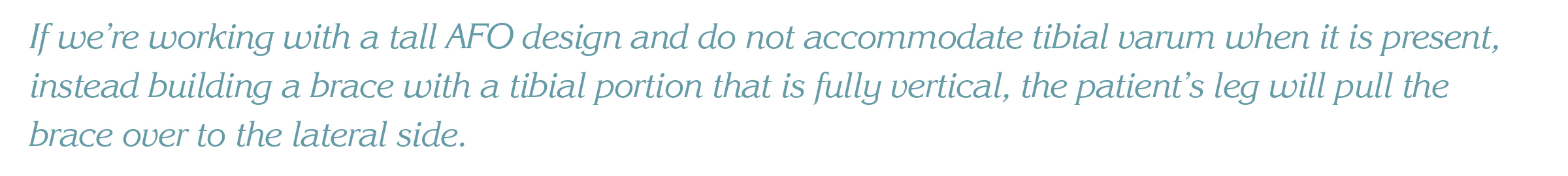
Now think of how gait happens for a person wearing a brace. For an excessive pronator, when the heel and tibial angle are both vertical, the leg in a vertical brace helps to create a more stable base during the moment of greatest weight-bearing (mid-stance), because the brace pulls the walker away from an excessively pronated position. For an over-supinator, though, shifting a fully vertical AFO laterally to match the natural alignment of the lower leg would not be beneficial. Instead, it would result in greater instability just when the walker would be moving into mid-stance and full weight bearing. The brace would be in contact with the ground only on the lateral edge of the plantar surface. (See Image 2, next page.)
The lesson, in regard to gait, is that hindfoot verticality should be in reference to the horizontal surface at mid-stance, rather than in reference to the tibial angle.
Planning the position of function
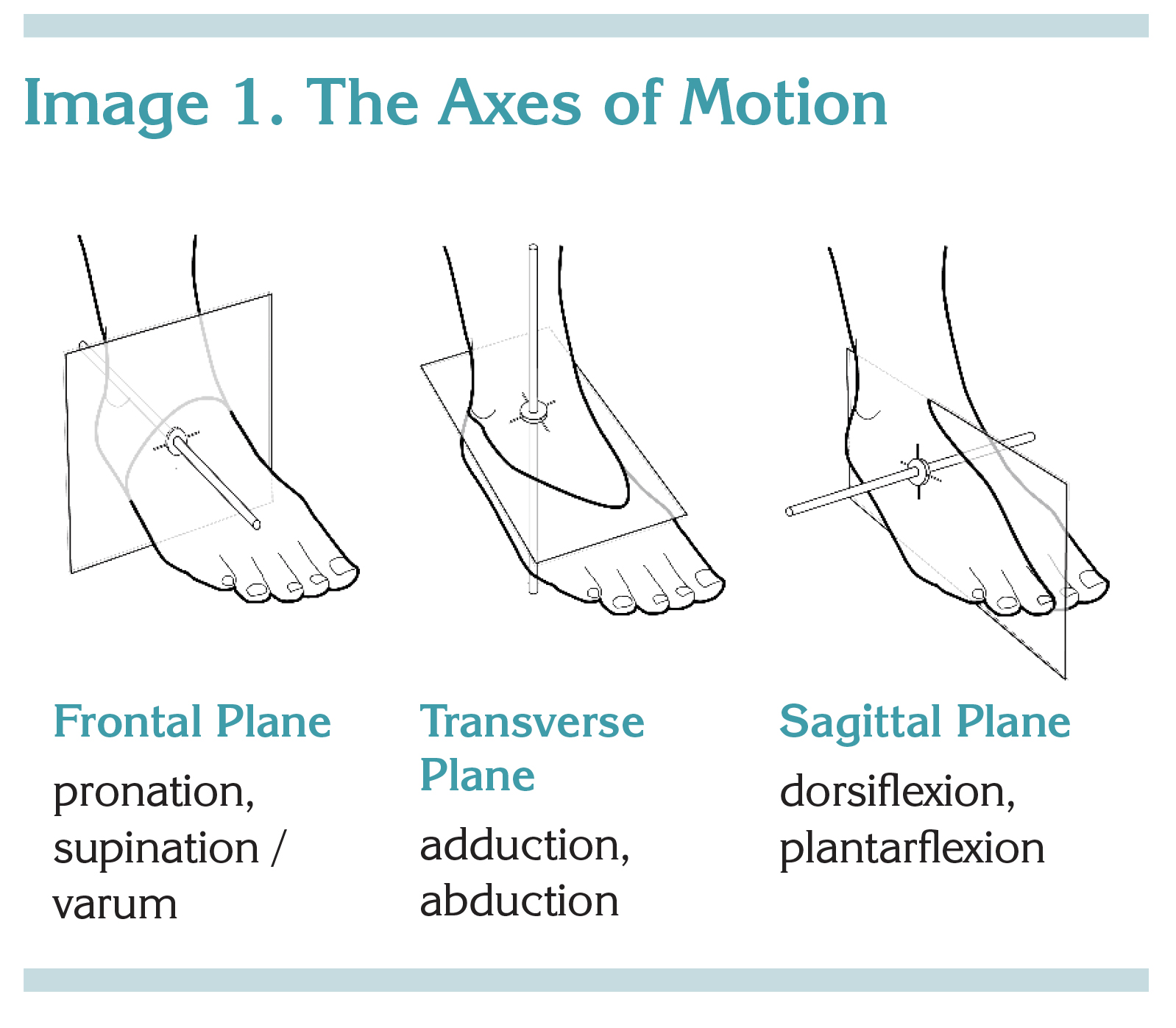 When developing bracing goals, we at Cascade typically plan an AFO to give the patient a functional foot and ankle position at midstance. Assuming the patient has sufficient range, our desired position of function includes a tri-plane consideration of the foot and ankle. We aim for (1) hindfoot vertical and forefoot level (frontal plane), (2) forefoot and hindfoot aligned (that is, neither adducted nor abducted; transverse plane), and (3) ankle dorsiflexion (DF) at 3 degrees (sagittal plane).
When developing bracing goals, we at Cascade typically plan an AFO to give the patient a functional foot and ankle position at midstance. Assuming the patient has sufficient range, our desired position of function includes a tri-plane consideration of the foot and ankle. We aim for (1) hindfoot vertical and forefoot level (frontal plane), (2) forefoot and hindfoot aligned (that is, neither adducted nor abducted; transverse plane), and (3) ankle dorsiflexion (DF) at 3 degrees (sagittal plane).
Such a foot and ankle position gives the patient mechanical efficiency by balancing between pronation and supination. This position is stable and useful throughout the stance and swing phases of gait.
 The balanced foot position also allows good sensory information during the weight bearing portions of gait and stance. Full contact allows sensitive nerve endings on the plantar surface of the foot to respond as the pressure moves (1) across the bottom of the heel, (2) along the foot’s lateral border, (3) across all five metatarsal heads, and (4) under all five toes. This accompanies the gait movement from heel contact through midstance and into swing.
The balanced foot position also allows good sensory information during the weight bearing portions of gait and stance. Full contact allows sensitive nerve endings on the plantar surface of the foot to respond as the pressure moves (1) across the bottom of the heel, (2) along the foot’s lateral border, (3) across all five metatarsal heads, and (4) under all five toes. This accompanies the gait movement from heel contact through midstance and into swing.
When the ankle is dorsiflexed 3 degrees in the sagittal plane, the ankle configuration is what influences the forward movement of the center of pressure from a patient’s heel to forefoot. This allows pressure on the foot to move as described in the gait section.
When tibial varum is present, this typical position of function becomes more complex. To look again at the mid-stance/full weight bearing stage of the gait cycle, if we’re working with a tall AFO design and do not accommodate tibial varum when it is present, instead building a brace with a tibial portion that is fully vertical, the patient’s leg will pull the brace over to the lateral side. The foot section, because it is connected to the proximal part of the brace, will follow. In a supinating patient, this will result in a supinated foot position, the very thing we’re trying to change. This will also unravel our lofty goal—providing a solid base of support by bringing the plantar surface into a balanced, full-contact position.
In contrast, for pronators, a little supination will counter the tendency to over-pronate so that if tibial varum is present yet goes unnoticed, it may not have as much of a negative impact on the overall project.
Accommodating tibial varum
We learned, from considering all of these dynamics, that the midstance angle of the patient’s limb needs to be set into the brace. Therefore, rather than evaluating a cast (or brace) by looking for verticality, it’s best to set it on a horizontal surface, imagine the lateral angle of the lower leg at mid-stance, and look for the mid-stance foot position. In a foot that is correctable to a balanced position, you should see a vertical to slightly everted heel and level forefoot. The distal end of the tibial portion of the cast or brace may be closer to midline than the proximal end, and that’s okay, when it respects a patient’s true tibial alignment.
Since stability is set mostly at full weight-bearing, the key for mobility is good stability at that point. The key to mobility—for effective coordination and movement of the airborne leg—is stability on the weight-bearing side. It’s the weight bearing leg that allows for her forward limb progression in swing, and it has a greater share in determining gait than the contralateral side. Given the general tendency to look mostly at swing phase issues, this feels like a breakthrough to me.
It’s also important to note that a typical leg in swing phase, if relaxed, is generally in slight supination. The bigger observation is that walkers do not move in perfect verticality all through the gait cycle. We oscillate between pronation and supination, twisting in a transverse spring-like motion that allows our pelvis and hips to propel the airborne leg.
 Don Buethorn, CPO, is founder-owner of Cascade Dafo, Inc. and Cascade Prosthetics and Orthotics.
Don Buethorn, CPO, is founder-owner of Cascade Dafo, Inc. and Cascade Prosthetics and Orthotics.